The Current Perspectives of Palliative Care
Last Monday, Dr. Linda Sutton gave a speech on palliative care at the National Comprehensive Cancer Network Summit on Patient Advocacy. A subset of healthcare commonly misunderstood, palliative care is no longer just end-of-life care.
What is palliative care? How is it different from hospice?
Dr. Sutton: There are many definitions of palliative care –CMS’ [Center for Medicare and Medicaid Services] is based on how palliative care is paid for; while the World Health Organization’s, is broad and inclusive but complicated and characterized by what palliative care is not. The definitions that have made the most sense to me and my patients are those definitions that emphasize what palliative care does – alleviate the multi-dimensional suffering of patients with serious and chronic illnesses.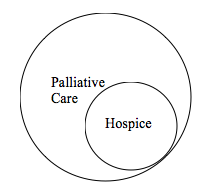
One way to help explain the difference between palliative care and hospice is to use a diagram:
All care provided by hospice is palliative care, but only a small proportion of all the palliative care provided is hospice care. Hospice is largely defined by the CMS criteria for eligibility; most notably that patients have a life expectancy of 6 months or less if the disease runs its usual course. That has largely limited the applicability of hospice. Palliative care is not constrained by how insurance companies or Medicare define the care.
Why does this misconception exist with palliative care?
Early on, as palliative care emerged as a medical specialty in its own right, the effort was to distinguish palliative care from other disciplines and approaches. Palliative care advocates spent a lot of time and energy emphasizing what palliative care was not; rather than focusing on what it was. Some of this was driven by the negative connotation of ‘hospice.’ The unfortunate reality is that hospice care is inextricably linked to dying. Hospice provides terrific palliative care that focuses on the patient and the family as the unit of care, but does so explicitly for those who are dying. Palliative care advocates wanted to offer that care to others, who might not be dying, but still faced high levels of stress – both physiologic and psychosocial due to serious medical illness(es).
How do you think we can change the perception of palliative care?
I think the only ways to change perceptions are through education and experience. Clearly more education of both our clinical providers and the public in general is required. But, what will be more important, in the final analysis, is what experiences do patients and their families have with palliative care? If good patient experiences are shared, more people will know about and seek help from palliative care specialists. However, it will be a challenge to significantly increase patient experience over the next few years, given the shortage of clinicians skilled in palliative care.
Do most doctors know the benefits? Or do you need to see a specialist?
I am not convinced that most physicians yet see how palliative care specialists can help their patients. In many locations or places of practice, there is not a palliative care specialist immediately available – the closest specialist may be hundreds of miles away. That is important because a large proportion of the populace in need of palliative care really cannot travel to see a specialist due to the burden of their disease or illness. One consequence of this is that, if physicians cannot see the benefits of palliative care first-hand, it is difficult to understand how their own patients might be helped. Furthermore, much of the palliative care services that are offered are inpatient services and not available for outpatients. With fewer doctors going to the hospital on a regular basis to see patients, they again miss the opportunity to see the benefit of palliative care services.
We may need to develop more creative ways of delivering palliative care – perhaps using telemedicine or other technologies.
Do all patients who need palliative care require a ‘palliative care specialist’?
This is complicated, because no two patient situations are alike. But, I don’t think ALL patients with serious illness need palliative care but they should have access to clinical providers with training in palliative care – that might be a social worker, or nurse specifically trained to address the palliative needs of patients. A good clinician working with others trained in palliative care –even if the clinician is not ‘board certified’ in palliative care, can alleviate significant amounts of patients’ distress.
If you think that you or someone you love needs palliative care, what is the first step toward getting it?
Always, start with your physician. Contact your local hospital, if there are palliative care specialists in your community, they are likely on staff at your local hospital. Your local hospice might also have a palliative care specialist on staff as well or can help with locating those resources.
Did you know that palliative care wasn’t just end-of-life care? Would you consider it for yourself or a loved one, or is this misconception still too strong? Tell us about your views on palliative care, and if it changed, in the comments section!